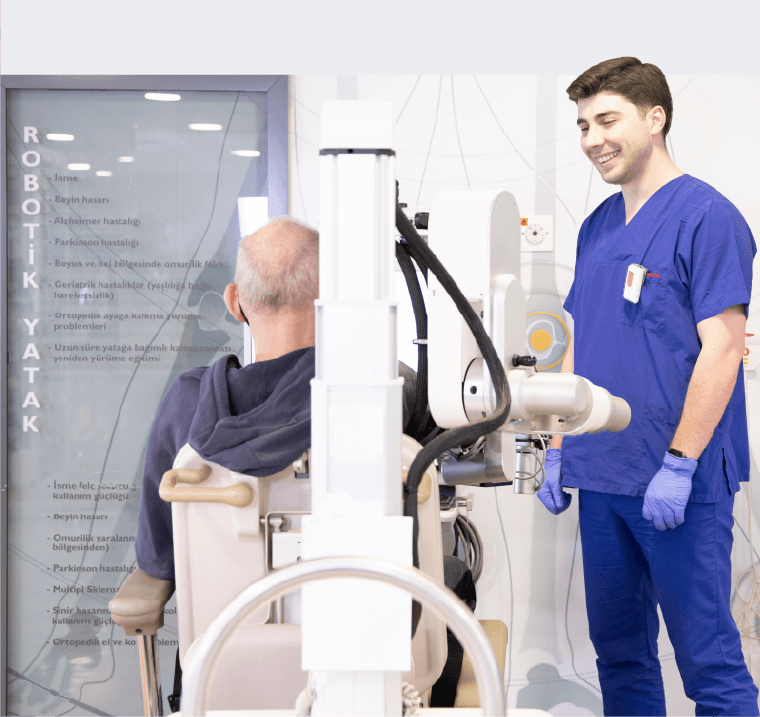
“16 yaşındayken 2 defa beyin kanaması geçirdim ve felç kaldım. Uzun süre yoğun bakımda yattım. Yaşamama mucize olarak bakılıyordu. Pes etmedim ve iyileştim, şimdi üniversiteye başlamanın heyecanını yaşıyorum… Benim 2 süpermenim var. Birisi ablam; beni doğru hocaya ulaştırdı. İkincisi de beni bu hale getiren Engin Hocam.”